My name is Myrtha and I am a
graduate student in the Biology Department at Western Illinois University. I am
currently working with Dr. Richard Musser on the genetic expression of
caterpillars that feed on Maize plants treated with the fungus Phialocephala fortinii. Taking medical
mycology with Dr. Porras-Alfaro has exposed me to a variety of fungus and I have gained essential knowledge that I am able to apply to my current research. In this
blog I will introduce you to an interesting fungi Lacazia loboi.
Lobomycosis:
Lacazia loboi
Taxonomy
Domain: Eukaryote
Kingdom: Fungi
Phylum: Ascomycota
Order: Onygenales
Genus: Lacazia
Species: loboi
(only known species)
General description
Lacazia loboi is a fungal pathogen and the causative agent of an
infection called lobomycosis. Lobomycosis commonly called lacaziosis, Jorge’s
Disease, and Jorge Lôbo’s Disease is a chronic disease that affects humans and
dolphins following traumatic injuries to the skin (2, 6, 7). The disease can
manifest as cutaneous or subcutaneous lobomycosis characterized by smooth,
verrucoses, or ulcerated nodules on the ear lobes and limbs in humans; on the
head, flippers, flukes, dorsal fin, and peduncle in dolphins (2, 6, 8).
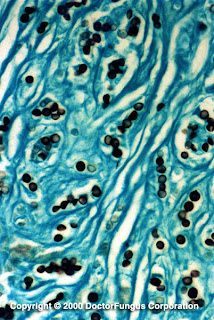 | |
| Fig 1.Stained tissues infected with Lacazia loboi (Doctor fungus) |
Lacazia
loboi has been given various names over the years such as Glenosporella loboi, Glenosporosis
amazonica, Lobomyces loboi and Loboa
loboi (5, 9, 11). Humans and a few species of dolphins, Tusiops truncates and Sotalia guianensi,
are the major hosts of this disease (4). Lobomycosis seems to affect older
population of dolphins with immunosuppressed systems (2). Although the disease
shows similar symptoms in humans and dolphins, microscopic shows some morphological
differences in the size of the lesions and the destruction of the cell. The fungal structures
that affect human are significantly larger than those that affect dolphins (5).
 |
Fig. 2 Verrucoid lesions on a person infected with Lacazia loboi
http://www.mycology.adelaide.edu.au/Mycoses/Subcutaneous/Lobomycosis/
|
 |
| Fig 3. Dolphin showing signs of
lobomycosis
(http://wwwnc.cdc.gov/eid/article/15/4/08-1358-f2.htm)on |
Distribution
Lacazia
loboi is found in tropical regions such as Brazil, Bolivia, Colombia, Costa
Rica, Guyana, Ecuador, French Guiana, Mexico, Peru, Panama, Surinam, and
Venezuela (1, 6, 8). The endemic regions are humid, with large forests and
rivers, and have over 200 cm of rain annually (9). Several human cases have also been reported in
Holland, Bangladesh, Canada, the United States in Florida and Georgia (1, 3). And the few individuals infected reported
traveling in the endemic areas several years preceding the onset of the disease
(1). Numerous cases of L. loboi in dolphins have been reported in several
areas of Florida (Gulf coast, Vero Beach, the Atlantic coast and Marineland)
and the Surinam River estuary, the Spanish-French coast, the south Brazilian
coast, the Indian River Lagoon, and the Texas coast of the Gulf of Mexico (10).
Habitat
Lacazia
loboi’s natural reservoir is
still unknown, though its occurrence in dolphins led researchers to believe
that L. loboi lives in aquatic
environments (8, 12). Based on the results of molecular testing it is known that L. loboi is indeed a dimorphic
fungus that exists as a hyphae in nature (7).
Look Alikes
Paracoccidioides brasiliensis and L. loboi share similar yeast-like cells.
Due to the presence of melanin in the cell wall of L. loboi it was thought to be related to the black fungi Cladosporium sphaerospermum (6).
Case study 1
A
42-year-old male from Georgia came to a general surgeon with a raised 3.5 by 2
cm smooth nodule on his chest. The nodule appeared reddish purple surrounded by
keloidal scar tissue. The biopsied tissues were stained and examined
microscopically (1). The results showed:
-
inflamed infiltrate of foamy histiocytes with globose and subglobose
lemon-shaped budding cells with diameter between 5 to 11 μm.
-
narrow tubular connections between daughter and
mother cells.
-
multinucleated giant cells
-
scattered lymphocytes
The patient reported traveling to Venezuela,
one of the lobomycosis-endemic countries a few years prior to the onset of the
disease.
Treatment:
The patient was treated by excising the lesion via an uncomplicated procedure.
It was reported that the patient recovered fully (1).
Click on this link http://www.ncbi.nlm.nih.gov/pubmed/10699043
for more information on the case.
Case study 2
A 42-year-old female from Canada
presented to her doctor with a plaque-like lesion on her upper right arm. The
lesion appeared red with a diameter of 1.5cm surrounded by keloidal scar tissue and
emerged on the same spot where a lesion was removed a few years earlier. The
patient not only travelled to lobomycosis endemic regions such as Mexico, Costa
Rica but also lived in Guyana and Venezuela for 2 years. Biopsied tissues taken
from the patient were stained and examined (3). The results showed:
-
multinucleated giant cells
-
thick-walled and spherical or lemon-shaped
budding cells with a diameter of 10 μm
-
Cells were in chains and joined by narrow
tubular connections
Treatment:
The lesion was excised and the patient recovered completely (3).
Click on this link http://wwwnc.cdc.gov/eid/article/10/4/pdfs/03-0416.pdf
for more details on the case.
Case study 3
Two cases of lobomycosis in bottlenose dolphins (Tusiops truncates) in North Carolina. The first dolphin, a male Atlantic bottlenose, was found dead on the North Carolina coast. Multiple areas of the dolphin’s skin were covered with raised, ulcerated, and papillary nodules, and cutaneous lesions (10).
Two cases of lobomycosis in bottlenose dolphins (Tusiops truncates) in North Carolina. The first dolphin, a male Atlantic bottlenose, was found dead on the North Carolina coast. Multiple areas of the dolphin’s skin were covered with raised, ulcerated, and papillary nodules, and cutaneous lesions (10).
 |
| Fig. 4 A. Serpigenous dermal
nodules on a dolphin. B. Microscopic view of spherical fungi connected to each other |
Microscopic stains of the lesions revealed:
-
cutaneous and subcutaneous nodule with
giant cells
giant cells
-
lymphocytes
-
plasma cells
-
epithelioid macrophages
-
spherical fungi with diameters between 6 and 10 μm connected to each other by small tubules.
The second dolphin was a live male
and was also found in North Carolina. Dermal nodules enclosing fungal yeast
like structures (10).
Treatment: No
treatment was listed for this case study.
Click on this link http://wwwnc.cdc.gov/eid/article/15/4/08-1358_article.htm
for more details on the cases.
Glossary
Histiocytes: multinucleated
giant cells
Keloidal scar: is
a result of an overgrowth of tissue at the site of skin injury.
References
1. Burns, R.A., Roy, J. S., Woods, C., Padhye, A.A.,
Warnock, D.W. (2000). Report of the first human case of Lobomycosis in the
United States. Journal of Clinical Microbiology. 38(3): 1283-1285.
2. Durden, W.N., St. Leger, J., Stolen, M., Mazza, T.,
Londono, C. (2009). Lacaziosis in bottlenose dolphins (Tursiops truncates) in the Indian river Lagoon, FL, USA. Journal of
Wildlife Diseases. 45(3): 849-856.
3. Elsayed, S., Kuhn, S.M., Barber, D., Church, D.L., Adams,
S., Kasper, R. (2004). Human case of Lobomycosis. Centers for Disease Control
and Prevention. 10(4).
4. Hart, L. (2009). The prevalence and progression of
lobomycosis in Sarasota Bay dolphins. Health and Physiology. Retrieved from
http://wwwnc.cdc.gov/eid/article/15/4/08-1358_article.htm 3/4/2013.
5. Haubold, E.M., Cooper Jr., C.R., Wen, J.W., McGinnis,
M.R., Cowan, D.F.(2000). Comparative morphology of Lacazia loboi (syn. Loboa
loboi) in dolphins and humans. Journal of Medical Mycology. (38): 9-10.
6. Herr, R.A., Tarcha, E.J., Taborda, P.R., Taylor, J.W.,
Ajello, L., Mendoza, L. (2000). Phylogenetic analysis of Lacazia loboi places
this previously uncharacterized pathogen within the dimorphic Onygenales.
Journal of Clinical Microbiology. 39(1): 309-314.
7. Mendoza, L., Ajello, L., Taylor, J.W. (2001). The
taxonomic status of Lacazia loboi and
Rhinosporidium seeberi has been
finally resolved with the use of molecular tools. Revista Iberoamericana de
Micología. 18: 95-98.
8. Murdoch, M.E., Reif, J.S., Mazzoil, M., McCulloch, S.D.,
Fair, P.A., Bossart, G.D. (2008). Lobomycosis in Bottlenose Dolphins (Tursiops truncates) from the Indian River
Lagoon, Florida: Estimation of
prevalence, temporal trends, and spatial distribution. International
Association for Ecology and Health. 5: 289-297.
9. Reiss, E., Shadomy, H.J., Lyon, G.M. 2012. Fundamental
Medical Mycology. New Jersey, NY: John Wiley & Sons, Inc.
10. Rotsein, D.S., Burdett, L.G., McLellan, W., Schwacke,
L., Rowles, T, Terio, K.A., …Pabst, A. (2009). Lobomycosis in offshore
bottlenose dolphins (Tursiops truncates), North Carolina. Emerging Infectious
Diseases. 15(4):588-590.
11. Taborda,
P.R., Taborda, V.A., McGinnis, M.R. (1999). Lacazia loboi gen. nov., comb.
nov., the etiologic agent of
Lobomycosis. Journal of Clinical Microbiology. 37 (6): 2031-2033.
12. Vilela, R.,
Mendoza, L., Rosa, P.S., Belone, A.F.F.B., Madeira, S., Opromolla, D.V.A., de Resende,
M.A. (2005). Molecular model for studying the uncultivated fungal pathogen Lacazia loboi. Journal of Clinical
Microbiology. 43(8): 3657-33661.